
Our Science
The future of heart disease treatment is bold
Tenaya is using biological insights from our team and our collaborators to discover novel therapies for various forms of heart disease, the leading cause of mortality worldwide. We are advancing a pipeline of disease-modifying therapies developed using our product platforms and core internal capabilities to target defined sub-populations of patients with rare or highly prevalent forms of heart disease. As displayed below, each of our product platforms is designed to address different problems that have historically plagued the development of novel therapies for heart disease.
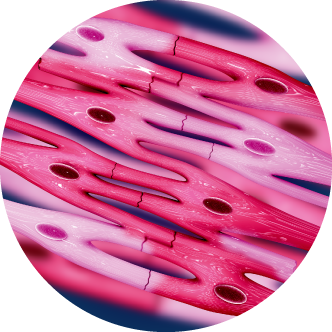
Cellular Regeneration
Problem: Heart cells that are lost (e.g. due to heart attack)
Tenaya Solution: Regenerate new heart cells in vivo by using viral vectors to deliver proprietary combinations of genes
Gene Therapy
Problem: Heart cells that are defective (e.g. due to mutations)
Tenaya Solution: Restore cell function by using viral vectors to deliver healthy copies of genes or other therapeutic payloads
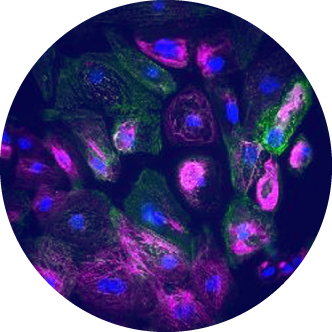
Precision Medicine
Problem: Lack of new targets with human validation
Tenaya Solution: Expand pipeline by using human iPSC-derived CM disease models and analysis of human genetics to identify new targets and therapies
Cellular Regeneration
Our Cellular Regeneration platform uses viral vectors to deliver genes to specific cells in the heart to regenerate cardiomyocytes in vivo. The product candidates arising from this platform are intended to overcome the shortcomings of traditional therapies that are not able to address the loss of cardiomyocytes. We believe this platform has the potential for broad utility across a range of heart conditions that result in the loss of cardiomyocytes, including myocardial infarction, chemotherapy-related toxicity, and viral infection.
Gene Therapy
Our Gene Therapy platform uses AAVs to deliver genes to specific cells in the heart to correct or compensate for functional defects. We have the ability to use both known AAV capsids as well as novel capsids identified through our internal capsid engineering capabilities to target cardiomyocytes, cardiac fibroblasts or other cells important to the proper functioning of the heart. The product candidates arising from this platform are intended to overcome the shortcomings of traditional therapies that are not able to address the underlying problems that contribute to heart disease. We believe this platform has potentially broad utility for both genetic and non-genetic forms of heart disease.
Precision Medicine
Our Precision Medicine platform uses human induced pluripotent stem cell-derived cardiomyocytes (hiPSC-CMs) as proprietary disease models and analysis of human genetics for the identification of new targets, validation of known targets, and high-throughput screening for drug discovery. This platform is intended to overcome the shortcomings of traditional drug development efforts that rely more heavily on efficacy in animal models to develop therapies intended for human heart disease. We believe this platform has potentially broad utility for the identification of targets and therapies in a modality-agnostic manner—including gene therapy, small molecules, and biologics—for both genetic and non-genetic forms of heart disease.
Drug Development Capabilities
We have internalized and integrated core capabilities to support our product platforms and our pipeline programs. We believe these capabilities can collectively support more rapid product development, precise delivery of our therapies to the heart, and more efficient and scalable manufacturing of our products. Taken together, these capabilities may ultimately improve the probability of technical and regulatory success of our product candidates that we hope to bring to patients who are fighting different forms of heart disease.
Disease Models
We have internalized the ability to create and integrate proprietary in vitro and in vivo models within our research organization. For our in vitro hiPSC-CM disease models, we use multiple methods to induce phenotypes within cell lines that simulate human diseases and then use these models for high throughput target identification and drug discovery. For our in vivo disease models, we have a dedicated onsite in vivo pharmacology group and vivarium, where we have established approximately 15 rodent heart disease models, both genetic and non-genetic, and can dose animals, perform heart surgeries, and use non-invasive imaging to assess the impact of our therapies under development.
Capsid Engineering
We have established in-house adeno-associated virus (AAV) capsid engineering capabilities and have successfully screened over one billion variants from more than 30 diverse, proprietary AAV libraries in multiple in vitro, in vivo and in silico models to discover novel AAV capsids that can target the different types of cells in the heart. These capsids are designed, and have shown in preclinical studies, to have desirable properties including the ability to more selectively target the heart versus other organs as well as lower susceptibility to neutralizing antibodies. We believe our capsid engineering efforts will be critical in supporting the successful clinical development of our product candidates and enabling those product candidates, if approved, to reach more patients.
Promoters and Regulatory Elements
We have created novel promoters and regulatory elements to support our gene therapy and cellular regeneration programs. We use these innovations to help ensure more precise and more robust expression of therapeutic payloads in the different cell types of the heart as compared to what can be achieved with currently available methods. We believe our innovations can support successful clinical development in part by improving the efficacy and safety profile of our product candidates.
Drug Delivery
We are actively exploring different routes of administration (ROAs) as well as different infusion- and injection-based methods for delivering our AAV-based therapies. We have designed a new catheter to support more targeted delivery and more efficient uptake of therapeutic payloads in the heart.
Manufacturing
We have established the Cardiac Genetic Medicines Manufacturing Center to support the production of our emerging portfolio of gene therapy and cellular regeneration product candidates. Tenaya’s state-of-the-art facility is designed to meet regulatory requirements for AAV-based gene therapies with initial capacity to produce current Good Manufacturing Practice (cGMP) drug product at the 1000L scale, utilizing Tenaya’s proprietary baculovirus-based production platform and suspension Sf9 cell culture system. The Center is located near our research labs in the San Francisco Bay Area to enable seamless collaboration across groups and is staffed by a growing in-house team with expertise in all aspects of gene therapy manufacturing, including process development (PD), analytical development (AD), quality assurance (QA) and quality control (QC).
Collaborations
Tenaya’s mission is to discover, develop, and deliver therapies that address the underlying drivers of heart disease. We were founded by leading cardiovascular scientists from, and have established academic collaborations with, Gladstone Institutes and University of Texas Southwestern Medical Center, and have forged additional partnerships aimed at helping advance our groundbreaking therapies. We are always open to strategic collaborations to push new boundaries in the treatment of heart disease.
For partnering inquiries, please contact us at partnering@tenayathera.com.


Publications & Presentations
Gene Therapy
TN-201 for MYBPC3-ASSOCIATED HCM
Differences in Patient Characteristics and Burden of Disease in Adults with MYBPC3-Associated HCM
2025 American College of Cardiology Scientific Sessions | Mar 31, 2025 Nature Communications | Mar 4, 2025 Hypertrophic Cardiomyopathy Medical Society (HCMS) Meeting | Sep 27, 2024Increased Disease Burden in Pediatric-onset MYBPC3-Associated HCM
2023 Hypertrophic Cardiomyopathy Medical Society (HCMS) Scientific Sessions | Oct 6, 2023 2023 Hypertrophic Cardiomyopathy Medical Society (HCMS) Scientific Sessions | Oct 6, 2023 HEART DEVELOPMENT AND DISEASE: FROM GENES TO CURES - 2023 KEYSTONE SYMPOSIA EVENT | Feb 12, 2023Modeling Hypertrophic Cardiomyopathy Due to MYBPC3 Haploinsufficiency with Engineered Heart Tissues
2021 Congress of the European Society of Gene and Cell Therapy | Oct 20, 2021 2021 American Society of Gene & Cell Therapy 24th Annual Meeting | Apr 27, 2021Reversal of Cardiac Hypertrophy with an Optimized MYBPC3 Gene Therapy
TN-401 for PKP2-ASSOCIATED ARVC
PKP2 Gene Therapy for Arrhythmogenic Right Ventricular Cardiomyopathy
Heart Rhythm Society Heart Rhythm 2022 | May 2, 2022 2021 Congress of the European Society of Gene and Cell Therapy | Oct 19, 2021Gene Editing (Discovery Stage)
Developing In Vivo Prime Editing as a Potential Treatment Option for Heart Disease
2025 ASGCT 28th Annual Meeting | May 14, 2025TN-501 Gene Editing Therapy for PLN-R14del-Associated Cardiomyopathy
2025 ASGCT 28th Annual Meeting | May 13, 2025 2024 American Society of Gene & Cell Therapy 27th Annual Meeting | May 10, 2024 2023 American Society of Gene & Cell Therapy 26th Annual Meeting | May 16, 2023Gene Editing of R14del Mutation in PLN Rescues PLN-R14del-Associated Cardiomyopathy
DWORF Gene Therapy For Heart Failure (Discovery Stage)
Developing A DWORF Micropeptide Gene Therapy For Heart Failure
Circulation Research | Oct 23, 2020Gene Therapy with the DWORF Micropeptide Attenuates Cardiomyopathy in Mice
ELife | Oct 9, 2018 Science | Jan 15, 2016A peptide encoded by a transcript annotated as long noncoding RNA enhances SERCA activity in muscle
Core Capabilities - AAV Capsid Engineering
Engineering Novel AAV Capsids for Cardiac Gene Delivery
2024 American Society of Gene & Cell Therapy 27th Annual Meeting | May 8, 2024AAV DNA Shuffle Library of GH Loop Regions for Directed Evolution of Cardiotropic Capsids
2024 American Society of Gene & Cell Therapy 27th Annual Meeting | May 8, 2024 2024 American Society of Gene & Cell Therapy 27th Annual Meeting | May 8, 2024Chimeric and Rationally Designed Compact Promoters for Cardiomyocyte-Specific Gene Expression
2023 American Society of Gene & Cell Therapy 26th Annual Meeting | May 16, 2023Engineering Novel AAV Capsids for Cardiac Gene Delivery
2022 EUROPEAN SOCIETY OF CELL AND GENE THERAPY 29TH CONGRESS | Oct 31, 2022Engineering Novel AAV Capsids for Cardiac Gene Delivery
2022 AMERICAN SOCIETY OF GENE & CELL THERAPY 25TH ANNUAL MEETING | May 17, 2022Engineering Novel AAV Capsids for Cardiac Gene Delivery
2020 American Society of Gene & Cell Therapy 23rd Annual Meeting | May 12, 2020Engineering Novel rAAV Vectors with Enhanced Cardiac Tropism
Core Capabilities - Genetic Medicines Manufacturing
Development of a Scalable High Yield HEK293 Expression Platform for AAV Manufacturing
2024 American Society of Gene & Cell Therapy 27th Annual Meeting | May 10, 2024 2023 American Society of Gene & Cell Therapy 26th Annual Meeting | May 16, 2023 2023 American Society of Gene & Cell Therapy 26th Annual Meeting | May 16, 2023 2023 American Society of Gene & Cell Therapy 26th Annual Meeting | May 16, 2023 2023 American Society of Gene & Cell Therapy 26th Annual Meeting | May 16, 2023Precision Medicine
TN-301 HDAC6 INHIBITOR SMALL MOLECULE
Targeting HDAC6 to treat heart failure with preserved ejection fraction in mice
Heart Failure Society of America (HFSA) Annual Scientific Meeting 2023 | Oct 6, 2023 Heart Failure Society of America (HFSA) Annual Scientific Meeting 2023 | Oct 6, 2023 Basic Cardiovascular Sciences Scientific Sessions 2023 | Oct 5, 2023 American Heart Association Scientific Sessions 2022 | Nov 5, 2022 SCIENCE TRANSLATIONAL MEDICINE | Jul 15, 2022 2022 EUROPEAN SOCIETY OF CARDIOLOGY - HEART FAILURE CONGRESS | May 24, 2022 2021 European Society of Cardiology - Heart Failure Congress | Jun 29, 2021 2021 European Society of Cardiology - Heart Failure Congress | Jun 29, 2021Phenotypic Screening Identifies HDAC6 Inhibitors as Cardioprotective Agents
Human iPSC-Derived Cardiomyocyte Screening
High-Throughput Imaging of Cardiomyocytes Using Biomimetic Tools Help Identify Therapeutic Targets
HEART DEVELOPMENT AND DISEASE: FROM GENES TO CURES - 2023 KEYSTONE SYMPOSIA EVENT | Feb 12, 2023 Basic Cardiovascular Sciences Scientific Sessions 2022 | Jul 26, 2022 eLife | Aug 2, 2021Cellular Regeneration
Reprogramming Cardiac Fibroblasts
Cardiac Direct Reprogramming Gene Therapy for Ischemic Injury
2020 American Society of Gene & Cell Therapy 23rd Annual Meeting | May 12, 2020Efficacy of Cardiac Reprogramming via Gene Therapy in Rat with Chronic Heart Failure
2020 American Society of Gene & Cell Therapy 23rd Annual Meeting | May 12, 2020Developing an Optimized Cardiac Reprogramming Cocktail for Gene Therapy in Humans
Transient Cardiomyocyte Proliferation
Transient Cell Cycle Induction in Cardiomyocytes to Treat Subacute Ischemic Heart Failure
Redox Biology | Aug 5, 2021Cell cycle induction in human cardiomyocytes is dependent on biosynthetic pathway activation
2019 American Heart Association (AHA) Scientific Session | Nov 19, 2019 Cell | Mar 22, 2018Regulation of Cell Cycle to Stimulate Adult Cardiomyocyte Proliferation and Cardiac Regeneration